Despite recent blogs on topics such as prescription opioid addiction, Zika virus and rising cesarean rates, the true heavyweight champion in the world of obstetrics has been, and remains, preterm birth (PTB). Seventy-five percent of non-anomalous infant deaths less than 1 year of age are a consequence of prematurity, not to mention billions of dollars in short and long-term health care costs.
To their continuing credit, the March of Dimes (MOD) embraced the challenge of reducing our nation’s high preterm birth rate with the initiation of their National Prematurity Campaign. After eradicating polio and supporting the researchers who discovered surfactant therapy for respiratory distress syndrome, the MOD decided to take on the elephant in the room. Despite initial tough sledding, the MOD has stuck to its agenda and has persisted in focusing its energy on reducing our national burden of premature delivery.
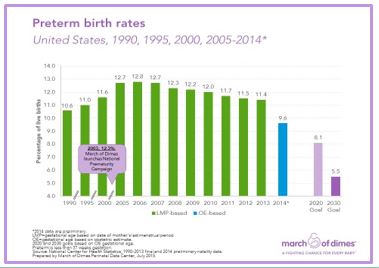
These efforts include an ambitious set of goals. The March of Dimes has established target goals to reduce preterm birth rates in the United States to 8.1% by 2020 and 5.5% by 2030. Many health care professionals are skeptical and believe achieving these targets are impossible in the United States. However, these same skeptics were pessimistic when the National Prematurity Campaign started in January 2003. As you can see from the graph above, these efforts have already reversed the pre-existing upward trend in PTB rates. Since the United States preterm birth rate peaked at 12.8% in 2006, there has been a progressive fall to a historically low rate of 9.6% in 2014.
All of a sudden, even skeptics are acknowledging that something unprecedented is happening. Again, it is an extraordinarily important obstetrical issue. If the 2030 MOD goals could be achieved, the result would be 1.3 million fewer preterm babies born between 2014 and 2030 and a savings of approximately $67 billion in health and societal costs.
So what are the components of the March of Dimes Prematurity Campaign Roadmap? While I’m sure that there are other contributors to prematurity prevention such as optimal nutrition and appropriate weight gain, adequate Vitamin D levels (>40 ng/ml) and avoidance of occupational fatigue, the MOD has identified the following seven interventions as critical. I do not argue with them.
- Eliminate non-medically indicated late preterm and early term deliveries-This is a part of the MOD “Give Me My 39” campaign to eliminate elective inductions and cesareans prior to 39 weeks of gestation unless there is a valid medical indication. This campaign has been dramatically successful in many, if not, most states including South Carolina. These statewide efforts have clearly reduced unnecessary late preterm births.
- Increase use of 17-alpha hydroxy progesterone (17-P) injections for women with a history of prior preterm birth- Only a minority of women who experience PTB also have a history of a prior PTB. However, their risk of recurrence is high and weekly 17-P injections can reduce that risk by about 40%.This is true for singleton, but not multiple gestations.
- Reduce tobacco use among pregnant women- Tobacco use is associated with both PTB and other complications such as placental abruption and fetal growth restriction. Approximately 10% of pregnant women still smoke and that number may be as high as 20% here in the Southeast.
- Space pregnancies at least 18 months apart- A short inter-pregnancy interval is a known risk factor for prematurity, as well as other maternal complications. Currently, about one-third of all deliveries occur within 18 months of the birth of a prior child.
- Use Low – Dose Aspirin to Prevent Pre-eclampsia – The etiology of pre-eclampsia is unknown. However, low dose or baby aspirin ( LDA) has been extensively studied as a preventative intervention. Meta-analysis of those studies have confirmed that LDA is safe and is probably associated with a modest 10-20% reduction in the risk of pre-eclampsia and fetal growth restriction. The U.S. Preventative Services Task Force recommends that all high risk women (prior history of pre-eclampsia or growth restriction, chronic hypertension or renal disease, diabetes, multiple gestations) should begin daily LDA as soon as pregnancy is recognized. This therapy is significantly underused.
- Identification and treatment of women with a short cervix- A short cervix in the mid-trimester (18-24 weeks’ gestation) is the strongest predictor of PTB, especially among women without a prior PTB history. The MOD is working towards universal mid-trimester screening of pregnant women for a short cervix which then allows them to take advantage of interventions that have proven beneficial in preventing PTB- namely, vaginal progesterone therapy, cervical cerclage and possibly a new vaginal pessary.
- Reducing multiple births through Assisted Reproductive Technology- Progress has been made with a dramatic reduction in triplet and higher order multiples by the reduction in multiple embryo transfers. Reducing twin births will require the broader adoption of a single embryo transfer policy with IVF and closer monitoring of ovulation induction cycles.
I truly believe that these and other interventions (see previous blog about the importance of optimal maternal nutrition in multiples), if aggressively pursued, can go a long way toward meeting these ambitious goals. However, even the MOD recognizes that meeting the 2030 goal of 5.5% will likely require the discovery of new, currently untested, therapies. Consequently, the MOD has invested $75 million/year to fund five major academic Prematurity Research Centers across the country whose mission is to investigate the diverse causes of PTB and explore potential new interventions. This new knowledge should contribute to new ways to identify and treat women at risk for preterm birth.
I don’t know if the MOD will achieve it’s goals. But, there is nobility in the effort and I look forward to tracking the success of that effort as we approach 2020 and beyond. We’re on the right track.
Preventing Prematurity-Related Morbidity:
Although, unlikely to contribute to a reduction in PTB rates, an important paper was recently published that should reduce prematurity-related morbidity. In the 1980’s, large clinical studies confirmed that antenatal corticosteroids reduced newborn respiratory disease and the risk of intracranial hemorrhage for infants born between 24 and 34 weeks’ gestation. This treatment has subsequently become standard of care.
Unfortunately, 70% of preterm births in the United States occur between 34 weeks 0 days and 36 weeks 6 days. In the past few months, Cynthia Gyamfi-Bannerman and colleagues at the Eunice Kennedy Shriver NICHD Maternal-Fetal Medicine Units Network published a trial in the New England Journal of Medicine examining the use of antenatal corticosteroids in women at risk for delivery in this late preterm period.
Study participants were women with singleton pregnancies who were anticipated to deliver between 34 weeks 0 days and 36 weeks and 5 days.Enrolled women were prospectively randomized to receive 2 doses (12 mg IM) of betamethasone 24 hours apart (1,429 women) or identical appearing placebo (1,402 women).
The use of betamethasone was associated with a significant 20% reduction in the primary outcome which was the need for respiratory support in the first 72 hours of life (14.4% placebo vs 11.6% betamethasone; p=0.02). Betamethasone was also associated with significant reductions in the incidence of severe respiratory complications, need for resuscitation at birth, need for surfactant therapy, incidence of transient tachypnea of the newborn and bronchopulmonary dysplasia. Late betamethasone exposure was associated with a greater risk of neonatal hypoglycemia (24% vs 15%; p<0.001).
These results are being rapidly introduced to clinical practice and should benefit thousands of babies being delivered in the late preterm time period. For the time being, the inclusion criteria used by the Antenatal Late Preterm Steroids (ALPS) study should be followed as our best evidenced-based medicine. Efforts should be made to follow the study conditions. Treatment is not indicated beyond 37 weeks’ gestation, steroids should not be repeated if previously given, delivery should not be delayed when indicated in order to give steroids, diabetics should be excluded, and the obstetrician should believe that at least 12 hours of ALPS can be achieved.
Thanks to the MOD, researchers supported by the NIH-NICHD, and many others, the hope is that the future with give every baby Born in the USA the best opportunity.