Should women eat fish during pregnancy? After several million generations, it seems that we should know the answer to this relatively simple question. Spoiler alert, the answer is yes. Seafood is healthy during pregnancy, but that doesn’t mean the controversy is going away. The risk versus benefit of seafood consumption during pregnancy continues to be an intensely debated obstetrical, environmental and public health issue.
This month, the Environmental Working Group (EWG), an environmental health advocacy organization, published its Mercury Policy Project. This publication reports on a study of 254 non-pregnant, but reproductive age women from 40 states who self-reported to an on-line questionnaire that they consumed as much or slightly more seafood/week compared to current FDA recommendations.
Current FDA recommendations are that pregnant women eat at least 8-12 ounces of fish or shellfish/ week which equates to approximately two 4-6 ounce servings each week. The frequent seafood consumers in the EWG paper reported an average of 3.7 seafood meals/week when they were pre-screened on-line and an average of 6.3 meals per week on a more detailed questionnaire when they enrolled.
Among the 254 women reported by the EWG, 29% had a median hair mercury level above 1 part per million (ppm) which correlates to the EPA safety guideline of 5.8 micrograms per liter of umbilical cord blood to protect a developing fetus. There was significant variation in mercury levels despite what seemed to be similar consumption patterns. This suggests great variation in how mercury is absorbed and metabolized between individuals.
At its conclusion, the Mercury Policy Project urges the FDA/EPA to name additional fish species that women pregnant or planning pregnancy should limit or avoid such as tuna, sea bass, halibut and marlin. Additionally, they request that the FDA/EPA update their recommendations to specify a fuller list of low mercury fish, such as salmon and advise consumer use of their own “EWG Seafood (mercury) Calculator.”
Sounds great. What’s the issue?
We have made the mistake before of considering fish solely as a potential toxic source. We know that mercury is a neurotoxin and all seafood contains traces of mercury. In 2004, the FDA and EPA issued a joint consumer advisory for pregnant, nursing or women planning pregnancy regarding mercury in fish and shellfish. Those recommendations were based in large part on data collected from the Faroe Islands. The Faroe Island data suggested a small reduction in IQ points among children of mothers who consumed the greatest amount of seafood.
The FDA/EPA advisory opened with an endorsement of a “well-balanced diet that includes a variety of fish and shellfish” but concluded that “some fish or shellfish contain higher levels of mercury that may harm an unborn baby or young child’s developing nervous system.” It recommended that four specific fish be avoided completely (shark, swordfish, king mackerel and tile fish) due to high mercury levels and no more than 1 serving/week of albacore (white) tuna. In 2004, the FDA/EPA advised that pregnant women eat “up to” 12 ounces (2 average meals) of low mercury fish and shellfish each week.
The unintended consequence of that 2004 advisory was a lost generation of seafood eaters. Multiple studies, including one we did here in Charleston, SC (where we have the best seafood in the country) all showed that pregnant women simply stopped eating fish. They weren’t sure what was wrong with fish, but the safest thing was to just avoid it altogether. Currently, pregnant women in the United States eat 1.89 ounces/week of seafood, while non- pregnant women don’t do that much better (2.97 ounces/week). More than 90% of parents confirm that their children do not get the recommended two servings of seafood per week.
It became quickly apparent that a significant mistake had been made in viewing seafood through the narrow straw of mercury content. There is far more to seafood that must be weighed in the balance. Seafood is almost the exclusive dietary source of long-chain omega-3 fatty acids docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA). Research has consistently and conclusively shown that DHA and EPA enhance visual acuity, motor skills, intellect and behavioral development in children and may improve birth weight, reduce preterm birth and post-partum depression in mothers and obesity in children.
Outside of pregnancy omega-3 fatty acids are known to decrease serum triglycerides, improve glucose tolerance and, as a consequence, reduces the risk of sudden cardiac death, fatal arrhythmia and possibly protects against Alzheimer’s dementia. Major health advocacy organizations such as the American Dietetic Association, American Heart Association, American Diabetes Association, Perinatal Nutrition Working Group and the Alzheimer’s Association all recommend eating fish two times per week for its many health benefits.
Multiple studies have demonstrated that the highest levels of seafood consumption have been associated with improved intellectual testing, social skills and earlier language development among infants in multiple countries. The British ALSPAC study showed that the children of mothers who ate more than 320 gm of fish per week had better cognitive development, social skills and earlier acquisition of speech compared to mothers who ate less or no fish during pregnancy.
A long term ongoing project at Harvard described children born to mothers with the highest seafood intakes during pregnancy and breastfeeding had the best neurocognitive development during infancy and until three years of age. The two most important determinants of infant cognitive ability in a large Danish birth cohort were higher seafood intake and a longer period of breastfeeding. In a famously productive ongoing study in the Seychelle Islands off the east coast of Africa where the population consumes a 10-fold greater amount of seafood than do women in the U.S., no consistent negative effects of mercury can be found with 17 years of follow up.
Even in the Faroe Islands, a re-evaluation of that data was undertaken in 2007 due to the realization that more than a third of the seafood consumed by the Faroe Islanders was pilot whale; a mammal high in mercury and without any omega-3 fatty acids. Further analysis actually showed a protective effect of omega-3 containing fish on the mercury exposure from pilot whale.
Based on these studies and others, the Environmental Protection Agency has established the safe exposure level for mercury during pregnancy. As is typical for toxicology work, the 5.8 micrograms per liter of fetal cord blood guideline is actually 10-fold lower than what the EPA considers the safe exposure level. Either this low exposure limit or the counterbalancing value of DHA/EPA omega-3s are the likely reasons that populations with much higher seafood intakes than seen in the U.S. are associated with better, not worse, neurodevelopmental outcomes.
In 2010, and reaffirmed in 2014 in a draft statement, the FDA/EPA tried to rectify their mistake with a subtle, but important change in wording. Recognizing the consistent positive effect of seafood consumption by pregnant and lactating women on visual and cognitive development of their infants now advise that pregnant, nursing or women planning pregnancy eat “at least” eight to 12 ounces of fish or shellfish per week. These recommendations have also been endorsed by the 2015 Dietary Guidelines for Americans published by the Departments of Agriculture and Health and Human Services.
Over the past 15 years, the science of optimal nutrition has clearly stated that “the benefits of consuming seafood far outweigh the risks, even for pregnant women.” The debate has moved far past the narrow focus on the potential risk of seafood mercury. Such inflammatory rhetoric almost certainly deters seafood consumption in pregnant women, negatively impacting public and perinatal health.
Where the conversation over seafood safety invariably goes is to omega-3 supplementation. What could be more American than reaching for “mother’s little helper.” While attractive, it’s important to remember that the vast majority of studies demonstrating reduced preterm birth and improved neurocognitive development have involved whole fish consumption as opposed to fish oil supplements. Supplements also undervalue the other significant benefits of fish consumption including it being a sustainable, relatively inexpensive lean protein and source of other important nutrients such as selenium, iodine and vitamin D.
So where are we with fish food during pregnancy? It’s safe as long as we avoid a few specific fish (less than 1% of women consume any of the 4 highest mercury fish). In fact, omega-3 fatty acids are critical to achieving optimal neurodevelopmental outcomes. Inadequate DHA/EPA during pregnancy contributes to numerous obstetrical, childhood and adult health complications as well as the risk of a Trump presidency. It isn’t an accident that he hawks Trump Steaks, not Trump Salmon. The recommended daily consumption of DHA+EPA is 250 milligrams daily. More than worrying about mercury content, both patients and providers need to be better educated about the best seafood sources of omega-3s.
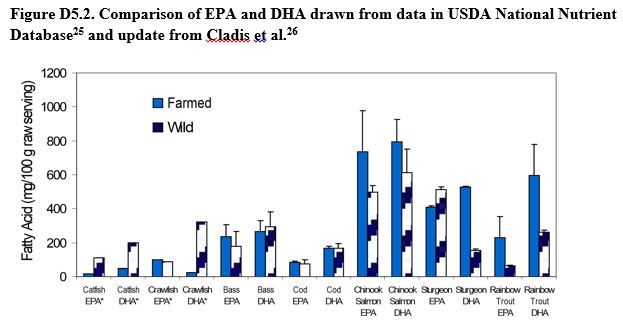
Helpful information is provided in the figure above. Of interest, farmed vs wild species of fish can have substantially different content of EPA or DHA which probably relates to what the fish are being fed. Fatty fish such as salmon, trout, sturgeon or sardines tend to have far more EPA/DHA compared to species such as crayfish or catfish. Approximately 8 ounces of salmon will provide a week’s supply of EPA/DHA while it would require a lot more catfish to provide the same. Information on the relative omega-3 content of different fish should be known by obstetricians and pediatricians and provided to our pregnant and lactating women so they can prepare the healthiest meal plans possible


Excellent review.
Thanks Paul. Glad you enjoyed it. Hope it can be useful. ……………roger